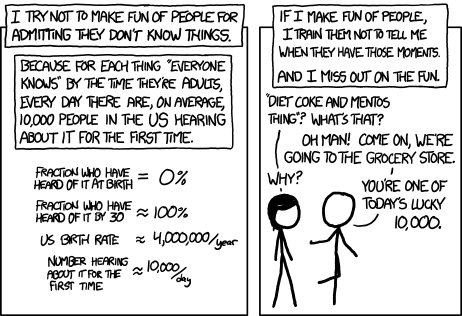
I was diagnosed with Type 1 diabetes over 15 years ago. During that time, I have had to learn a lot. A lot. Before eating any meal, I had to read food labels, calculate the total carbohydrates, and calculate the insulin dosing based on a personalised formula before injecting insulin. Sometimes I got it right. Sometimes I got it wrong. Eventually, I switched to an insulin pump which helped with more accurate dosing, but I still had to do a lot of math. A few years ago, manufacturers started combing insulin pumps with continuous glucose monitoring systems, something the press hyped as an artificial pancreas. They are NOT!
What they are is a closed-loop Automated Insulin Delivery System. AIDS automates blood glucose (BG) control as much as possible. The patient performs less frequent fingerstick blood glucose readings and is alleviated from calculating how much insulin to dose or reduce based on those readings. I have one of the first devices to be approved by the FDA. For many reasons, I think it’s a POS.
Fortunately, the warranty is ending on the device. I will be able to get a new device. Fortunately, more recent and more capable AIDS were approved in 2020. I took a look at a few of them and got excited about the Omnipod 5 Tubeless Automated Insulin Delivery System with Smartphone Control 5.
Our Diabetes Community now has the first-ever closed loop system that automates insulin delivery with no need for plastic tubing attached to your body. And this new system will be the first that is Food and Drug Administration (FDA)-cleared to be controlled by your smartphone.
...
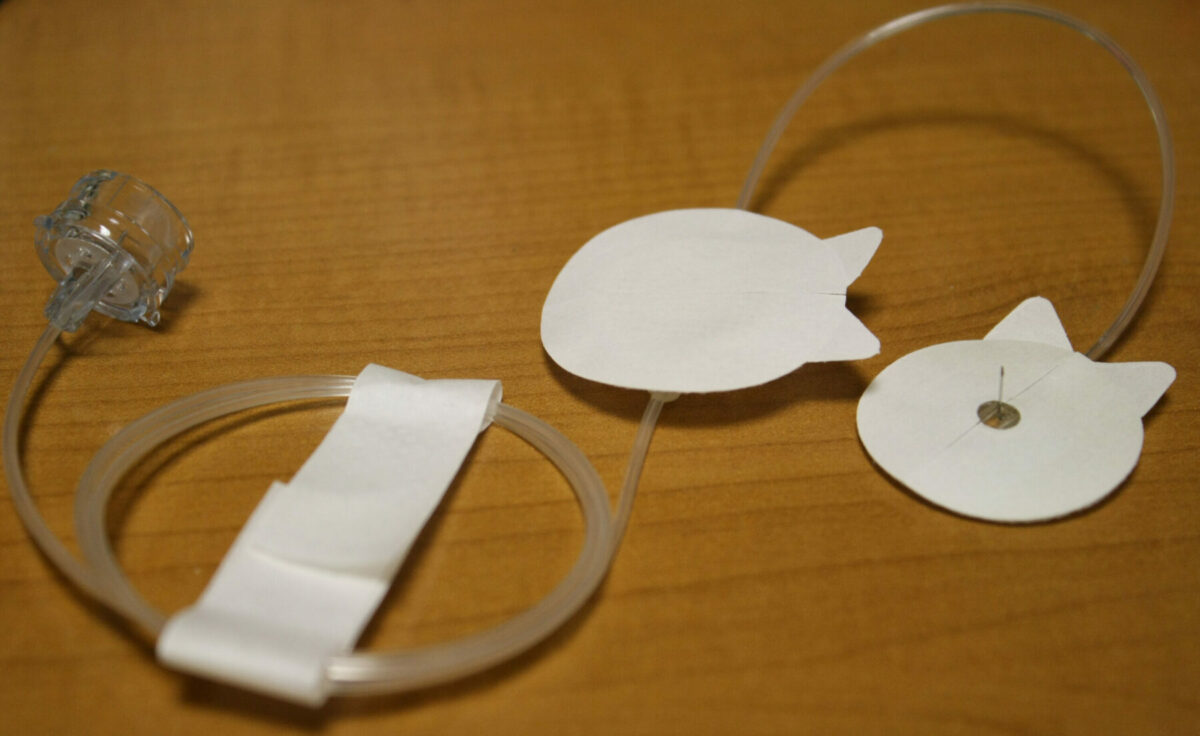
The new system combines the little white Omnipod patch pump with the Dexcom G6 continuous glucose monitor (CGM) and a controller algorithm to automate insulin delivery. Notably, Omnipod 5 makes history as the first such system to get FDA clearance for mobile app control and insulin dosing directly from your smartphone, eliminating the need to always carry a separate controller unit.
I sent a link to the Omnipod 5 "Patch" article to some friends. One of them responded with a few questions. In the process of answering his questions, I wrote this long-winded blog post.
Khurt, this sounds like great news, but how does the patch deliver insulin to you? Does it work on the same principle as the nicotine patch, which just gets absorbed into the skin?
Nature has had 500 million years to perfect homeostasis via the endocrine system. This is accomplished by a highly sophisticated network of hormones and neuropeptides released mainly from the brain, pancreas, liver, intestine, adipose and muscle tissue. Insulin, produced by a healthy pancreas, is just one of those factors. While these devices are welcome advances, they are crude stone-age tools compared to the human endocrine system. They can not control what happens once the insulin is injected into the body.
Banting discovered insulin nearly 100 years ago, but very little has changed human physiology. It is necessary to inject it directly into the body. Variability in insulin needs (every person has insulin needs specific to their body) and variability in skin absorption rates would produce too much unpredictability in insulin delivery if delivered via the skin. Absorption through the skin would make blood glucose control incredibly unreliable and extremely dangerous.
The Ominpod 5 Patch is not a patch like a nicotine patch. Insulin is a hormone, not a drug. Insulin is regulated on-demand in a person with a healthy pancreas and liver. In a person with T1D, the pancreas no longer produces insulin.
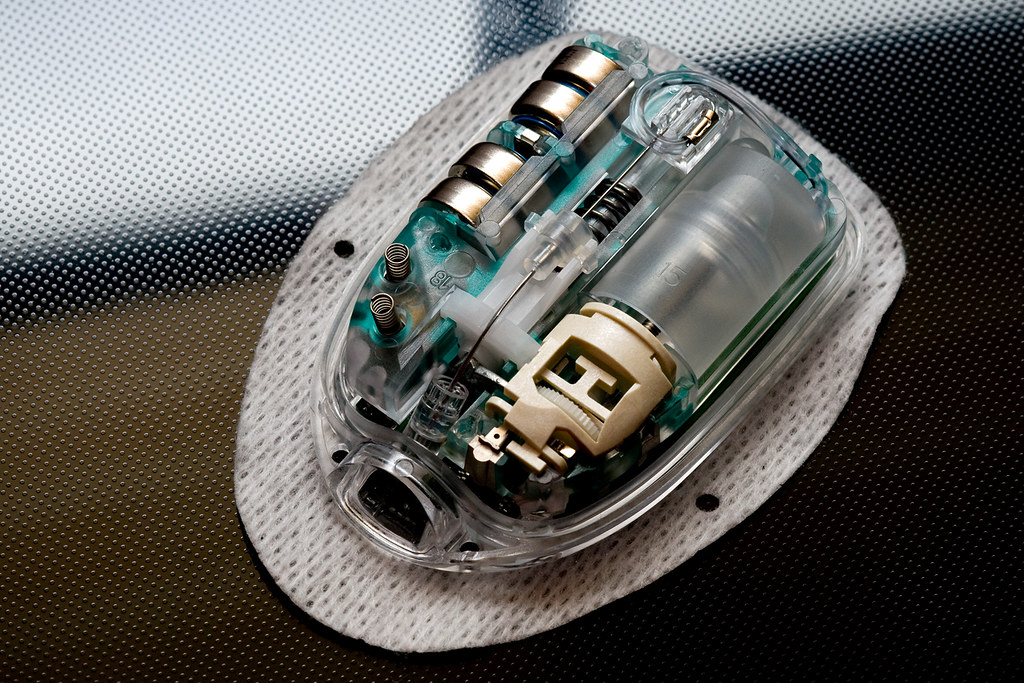
“Patch” is just Insulet Inc.'s branding for their product. The “Patch” is an insulin delivery device attached with adhesive to the body. The “Patch” contains a vial of insulin with a ¼ inch cannula (skinny needle) that gets inserted into the body. The device injects insulin into the body. The insertion site must be changed every three days to prevent infections and buildup of fat deposits.
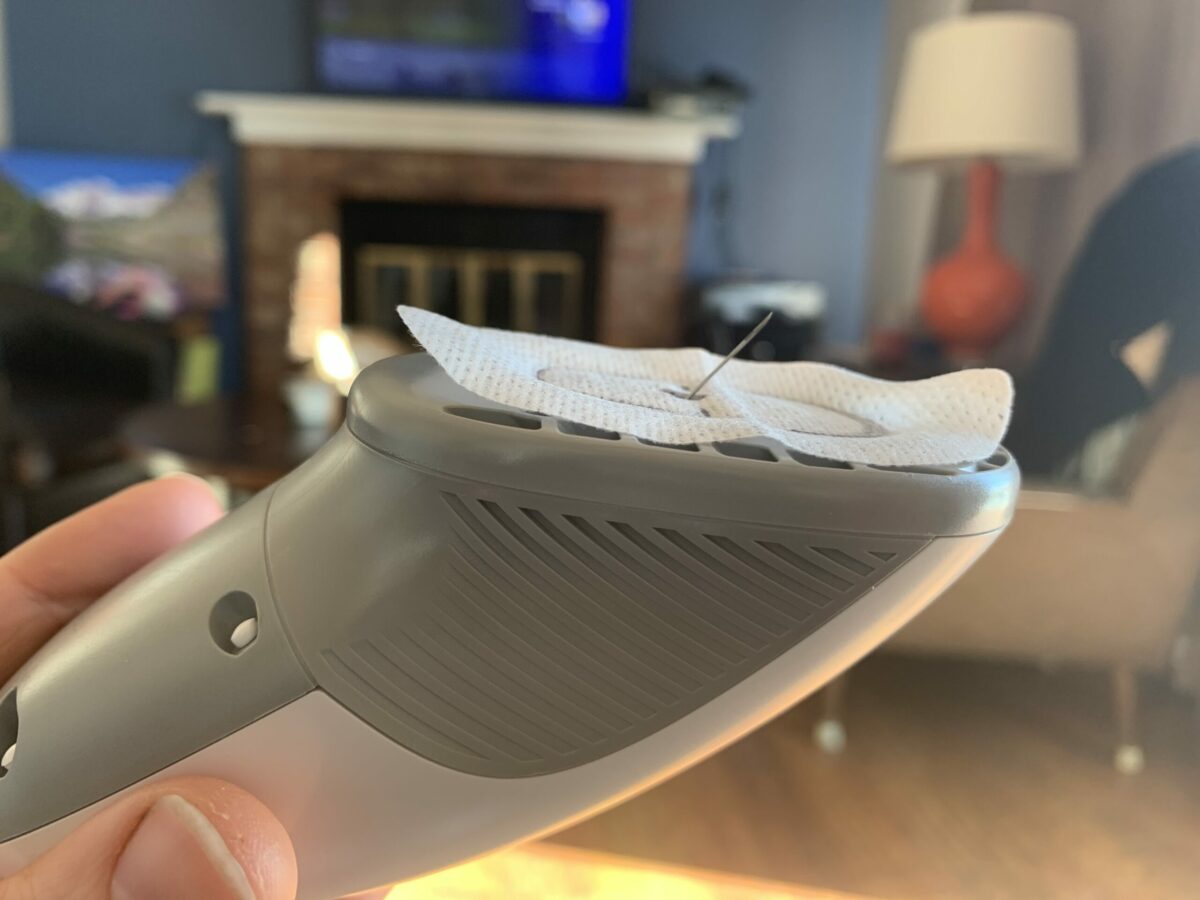
My current pump system and infusion set look like those in the photo below. Do you notice the tubing running from the insulin pump to a port on the body? I usually tuck the tubing into my pants with the pump on a clip to access the controls. But Dealing with all that tubing is a PITA. Sometimes it comes out, and I have had it snags on turnstiles and kitchen drawers. Sometimes it gets painfully yanked out. What Insulet Inc. have done is make an insulin pump that is attached directly to the body.

Can it deliver enough quickly in order to adjust to any spikes you may encounter, or is this something where you still may need needles to supplement in those cases, or would it require an even further adjustment to diet and avoid pizza and beer nights?
A spike in T1D means a rapid increase in blood glucose level over a 15-30 minute period. Despite what they portray in movies and TV shows, they don't happen in seconds. Since the Dexcom CGMS (Continuous Glucose Monitor System, a device separate from the insulin pump) sends blood glucose updates to the insulin pump every 5 minutes, the insulin pump algorithm can detect which direction blood glucose is trending and make adjustments to avoid spikes (or drops). Blood glucose spikes don’t pose any immediate health threat. Rapid declines in blood glucose may cause a person to blackout and go into a coma.

The CGMS has a ½ inch to 1-inch wire sensor inserted into the body. The insertion site must be changed every 5-7 days to prevent infections. Repeated studies have shown that accurate blood glucose levels are impossible without a blood sample. This is why I downplay hyped-up headlines about blood glucose testing via contact lenses (tears), smartwatches (looking through the skin) or other stupid ideas. They all proved too inaccurate for making a medical decision (i.e. how much insulin to inject).
Links for further reading:
- How Insulin Works In The Body
- How Does an Omnipod Insulin Pump Actually Work?
- What's Inside an Omnipod?
- Frederick Banting (1891–1941): Discoverer of insulin
- 'Artificial Pancreas' aka Automated Insulin Delivery: What You Should Know
- Omnipod 5: First Tubeless Automated Insulin Delivery System with Smartphone Control