Photo by Tanja Heffner on Unsplash
Having that thing go off, it's less about it going off every hour and asking me to stand for a minute, but of reminding me of the passage of time, that as a human being, I feed off of motion the same way that I feed off of food.
How often will the watch ask you to stand or move? If standing and moving intrude on my focused work effort which should win out? The stand/move or the focused concentration? What do I do if I am merely a participant in a 2-hour meeting with high-level executives? Do I just stand up in the middle of the meeting and walk out because my watch told me to?
Then linking that into, wow, I actually have more pain today. Tomorrow, I'm going to make more of a conscious effort to really pay attention to when the watch tells me to get up and move, and maybe have a walking meeting.
How do walking meetings work in practice? How easy is it to convince a group of people (or a single person) to go outdoors in very cold or very hot weather and work (think) while walking? What if one member of the group says no (perhaps they have a medical reason)? Does the other members of the team pile on in convincing that person to do a walking meeting?
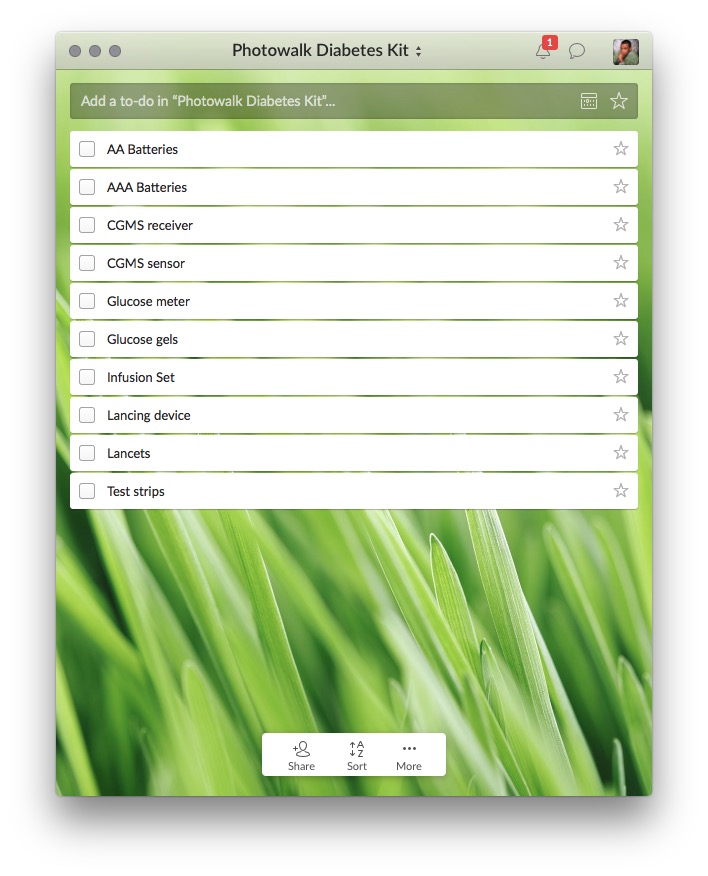
My wife just walked by while I was reading this article and suggested we go for a walk. I asked her if we could go in about 30 minutes. My Dexcom indicates that my blood glucose is 50 mg/dL. I need a glucose gel. If this had been a request for a walking meeting at a specific time I would have had to decline. For medical reasons that I would not want to explain to anyone.
Were you mindful when you were eating? Did you eat things that, at the end of the day, are going to balance out to cover all of the different nutrients you needed so that your body and your brain can function?
Yes. Sure. I have type 1 diabetes. I already do way more testing and monitoring and daily nutritional analysis than most people.
When we're talking about health and wellness with colleagues, with patients, or with clients, one of the things that we definitely do talk about is it's a buffet. It's rarely going to be a one-size-fits-all. It's really about paying attention to what it is that you need, and finding that best fit.
Truth!
A few of my friends and family have asked why I don't have an Apple Watch. They read some hyperventilating article about how Apple is working on a blood glucose monitor for diabetes. My Dexcom G5 CGMS is helping me do 24⁄7 blood glucose monitoring because of the ever-present risk of hypoglycemia because, like most people who have lived with Type 1 diabetes for a while, I have hypoglycemia unawareness. It's not a quantified lifestyle device toy.
Even if the Apple Watch could accurately monitor my blood glucose, it would need to be connected to me 24⁄7. My Dexcom transmitter battery last three months. Snapping in a new pre-charged transmitter takes two hours. The Apple Watch is good for 18 hours and needs to be connected to a charging stand to re-charge. This is nowhere near to being a replacement for my Dexcom G5.